Acute lymphoblastic leukemia: new insights into the biology of tumor development and persistence
Researchers at the University Medical Center Schleswig-Holstein (UKSH), Kiel Campus, identified molecular alterations in tumor stem cells that may precede acute lymphoblastic leukemia (ALL) and promote its persistence.
ALL is the most common malignant disease in children and occurs mainly between the ages of two to five. Adults also develop ALL, although much less frequently. This leukemia form originates from altered immature precursor cells of specific white blood cells, which cause reduced bone marrow function and impaired hematopoiesis and, if left untreated, lead to death.
With modern therapies, 90% of the affected children can now survive this disease – but only 40% of adults. Like many other cancers, ALL is characterized by changes in the genetic makeup of cells that can greatly affect the severity of the disease and thus its prognosis. Now, researchers from the CATCH ALL Clinical Research Group at UKSH Kiel in collaboration with the Max Planck Institute Plön, the University Hospital Frankfurt am Main and the Munich Leukemia Laboratory MLL showed that acquired changes in a specific gene can be observed in certain blood cells even after successful treatment. The results of the study were recently published in the scientific journal Blood.
Mutations in tumor suppressor genes occur even before the disease
For the study, researchers led by Dr. Dr. Guranda Chitadze, a scientist in the Clinician Scientist Program in Evolutionary Medicine, and Professor Monika Brüggemann, Section Head of the Hematology Laboratory Kiel of UKSH, examined blood and bone marrow samples from ALL patients for changes in a specific gene (TP53) over time from diagnosis to follow-up after therapy. Using modern molecular biology and immunology methods, they compared the mutation load of the TP53 gene in different cell compartments with the degree of so-called minimal or measurable residual disease (MRD).
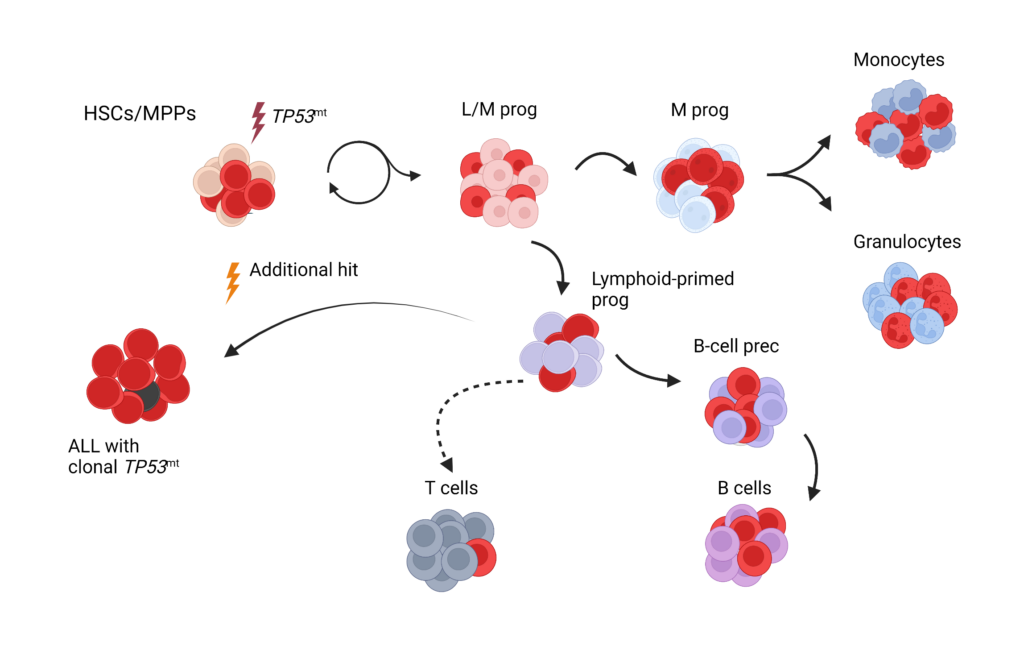
First author Guranda Chitadze, MD, Ph.D., explains, “It is known that mutations in the TP53 gene can be observed in approximately one-fifth of the patients with acute lymphoblastic leukemia. These mutations are associated with increased resistance to standard therapies and poorer survival.” For the study, 43 patients whose leukemia had TP53 mutations were retrospectively reviewed. About 70% of those affected could achieve molecular remission, meaning that certain disease markers were no longer detectable by molecular genetics. “Although minimal residual disease (MRD) was no longer detectable in these patients, we still detected mutations in the TP53 gene in about one-third of them,” Chitadze elaborates. Deeper analyses showed that changes in the gene were already found in blood precursor cells. Mutations in the TP53 gene may thus represent early events in pre-leukemic stages. Due to clonal proliferation of the cells, the mutations persist in the various hematopoietic cells, remain even during remission, and can lead to a disease recurrence.
“Our results provide substantial insight into the development of TP53-mutated ALL,” explains Professor Monika Brüggemann. “The findings could have important clinical significance for the choice of ALL therapy, monitoring of minimal residual disease, and the prediction for a treatment outcome. However, this will require further studies with a larger cohort in a prospective setting,” she emphasizes.
New leukemia therapy approaches for the clinic
This study is another result of the CATCH ALL Clinical Research Group, which has been funded by the DFG with around five million euros since the beginning of January 2022. Teams from research and clinic are working together to bring promising therapeutic approaches into clinical application. “The new findings can further contribute to optimize oncological precision diagnostics and therapy of acute lymphoblastic leukemia,” explains Professor Claudia Baldus, spokesperson of CATCH ALL. She emphasizes, “In general, we would like to improve the curing chances for all patients across all ages.”
Original publication:
Chitadze G, Stengel A, John-Klaua C, Bruckmüller J, Trautmann H, Kotrova M, Darzentas F, Kelm M, Pal K, Darzentas N, Bastian L, Kehden B, Wessels W, Ströh AS, Oberg HH, Altrock P, Baer C, Meggendorfer M, Gökbuget N, Baldus C, Haferlach C, Brüggemann M (2022): Somatic TP53 mutations are pre-leukemic events in acute lymphoblastic leukemia. Blood
First published: 30. November 2022, doi: 10.1182/blood.2022017249
Text: Dr. Claudia Taubenheim


